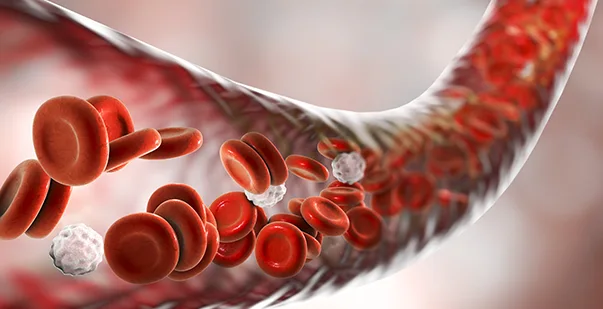
Hemostasis is the body’s natural defense mechanism against blood loss. This complex process involves various components working together to seal damaged blood vessels and prevent excessive bleeding. Recent research has shed light on the intricate molecular interactions that occur during hemostasis, enhancing our understanding of this vital physiological process.
Hemostasis is a multistep process that includes vasoconstriction, platelet plug formation, and blood clotting. These stages work together to stop blood flow from injured vessels and maintain the integrity of the circulatory system.
Read on to learn more about the hemostatic system, stages of hemostasis, affecting factors, and its clinical significance.
What is Hemostasis?
Hemostasis is defined as the body’s way of stopping bleeding when a blood vessel is injured. It’s a delicate balance between preventing blood loss and avoiding excessive clotting. The process involves several components of the blood and blood vessels working together.
Hemostasis, derived from the Greek words “heme” (blood) and “stasis” (halting), is a physiological process that maintains blood in a fluid state within intact blood vessels while also enabling rapid clot formation at sites of vascular injury. This intricate mechanism involves the coordinated action of blood vessels, platelets, and coagulation factors to prevent blood loss and maintain vascular integrity.
The process is essential for survival because it prevents excessive bleeding from small injuries. If the system is not functional in an organism, death could result from a small cut because of uncontrolled blood loss. On the other end of the spectrum, overactive hemostasis leads to blood clots and favors unwanted blood vessels that inhibit the movement of blood and are life-threatening conditions such as heart attack or stroke.
Stages of Hemostasis
The hemostatic process consists of several stages that work together to stop bleeding. Once you know what hemostasis is, you should also know its key stages. This process can be divided into four main stages:
- Vascular Spasm (Vasoconstriction)
Vascular spasms are the body’s immediate response to blood vessel damage. They are quick actions that help reduce blood flow to the injured area. This stage is crucial for initiating the hemostatic process.
When a blood vessel is damaged, the smooth muscles in the vessel wall contract immediately. This contraction narrows the blood vessel, reducing blood flow to the injured area. The spasm can last for several minutes, giving time for the next stages of hemostasis to take effect. Several factors contribute to this vasoconstriction:
- Norepinephrine: Released by the sympathetic nervous system, norepinephrine activates α-adrenergic receptors in blood vessels and promotes vasoconstriction.
- Endothelin: This is a potent vasoconstrictor produced by damaged endothelial cells, which is associated with injury-induced vessel constriction.
- Thromboxane A2 (TXA2): Released by activated platelets, this molecule promotes both platelet aggregation and vasoconstriction, particularly in injured tissues.
- Serotonin: Released by platelets during injury, serotonin causes vasoconstriction and reduces blood loss.
- Angiotensin II: A hormone that plays a key role in blood pressure regulation and fluid balance, it induces vasoconstriction, especially in response to decreased blood volume.
- Local Factors: In response to tissue metabolism, factors such as decreased pH and increased CO2 levels promote vasoconstriction to regulate blood flow and oxygen delivery.
While vasoconstriction is most effective in small blood vessels, it can significantly reduce blood loss and buy time for the formation of the platelet plug and blood clot.
First Aid Training Made Easy
Learn essential first aid care from anywhere with our online course
- Platelet Plug Formation (Primary Hemostasis)
Platelet plug formation, also known as primary hemostasis, is the second stage of the process. This stage involves the activation, adhesion, and aggregation of platelets to form a temporary seal at the site of injury.
Platelets are small, disc-shaped cell fragments that circulate in the blood. When a blood vessel is damaged, the underlying collagen fibers are exposed. Platelets have receptors that recognize and bind to these collagen fibers, causing them to adhere to the damaged area. The process of platelet plug formation involves several steps:
- Platelet Adhesion:
When the endothelium (inner lining of blood vessels) is damaged, platelets come into contact with exposed collagen and von Willebrand factor (vWF). They bind to these proteins using specific receptors on their surface, such as glycoprotein Ib (GPIb). Glycoprotein Ib (GPIb) is a receptor on platelets that binds to the von Willebrand factor, which is required in platelet adhesion during blood clotting
- Platelet Activation:
Once adhered, platelets become activated. They change shape from disc-like to spherical with protruding pseudopods, increasing their surface area. Activation also causes platelets to release the contents of their granules, which include ADP, serotonin, and thromboxane A2.
- Platelet Aggregation:
The released substances attract and activate more platelets. These newly activated platelets bind to the already adhered platelets, forming a platelet aggregate. Fibrinogen plays a crucial role in this step by binding to activated GPIIb/IIIa receptors on adjacent platelets, essentially bridging them together.
- Platelet Plug Consolidation:
As more platelets aggregate, they form a platelet plug that temporarily seals the break in the blood vessel wall.
While the platelet plug can effectively stop bleeding from small vessels, it’s not strong enough to stop bleeding from larger vessels or withstand high blood pressure. This is where the next stage of hemostasis comes into play.
- Blood Coagulation (Secondary Hemostasis)
Primary hemostasis (the initial response) involves the aggregation of platelets to form a temporary plug. Blood coagulation, or secondary hemostasis, is the process of forming a fibrin clot to stabilize the platelet plug. This stage involves a complex series of enzymatic reactions known as the coagulation cascade.
The coagulation cascade is a series of reactions where inactive enzyme precursors (zymogens) are activated sequentially. Each activated factor then activates the next factor in the cascade. This process amplifies the initial signal and results in the rapid formation of fibrin, the main component of a blood clot. Two pathways can initiate the coagulation cascade:
- Extrinsic Pathway:
This pathway is initiated when blood comes into contact with tissue factor (TF) exposed by damaged cells outside the blood vessel. It’s called “extrinsic” because the trigger (TF) comes from outside the blood.
- Intrinsic Pathway:
This pathway is activated when blood comes into contact with negatively charged surfaces, such as collagen in damaged blood vessels. It’s called “intrinsic” because all the factors needed are present in the blood.
Both pathways converge at the activation of Factor X, leading to the common pathway. This final series of reactions converts fibrinogen to fibrin, which forms the mesh of the blood clot. Thus, the key steps in the coagulation cascade include:
- Activation of Factor X to Factor Xa,
- Conversion of prothrombin to thrombin by Factor Xa,
- Conversion of fibrinogen to fibrin by thrombin,
- Cross-linking of fibrin by Factor XIIIa to form a stable clot.
The result is a fibrin mesh that reinforces the platelet plug, which creates a stable clot that can withstand the pressure of blood flow and effectively seal the damaged blood vessel.
- Clot Retraction and Fibrinolysis
Clot retraction and fibrinolysis are the final stages of hemostasis. These processes help to strengthen the clot and eventually remove it when it’s no longer needed. They’re crucial for wound healing and restoring normal blood flow.
- Clot Retraction:
After the fibrin clot has formed, it begins to contract or retract. The platelets in the clot drive this process. The platelets contain contractile proteins (actin and myosin) that can pull on the fibrin strands, causing the entire clot to shrink. Clot retraction serves several purposes:
- It pulls the edges of the damaged blood vessel closer together, aiding in wound healing.
- It makes the clot more compact and stronger, better able to withstand the pressure of blood flow.
- It squeezes out excess fluid (serum) from the clot, making it more solid.
- Fibrinolysis:
Fibrinolysis is the process of breaking down the fibrin clot. It’s an essential part of hemostasis because it prevents clots from growing too large and ensures they’re removed once they’re no longer needed.
The main enzyme responsible for fibrinolysis is plasmin. Plasmin is produced from its inactive precursor, plasminogen, which is activated by tissue plasminogen activator (tPA) and urokinase. The key steps in fibrinolysis include:
- Activation of plasminogen to plasmin,
- Degradation of fibrin by plasmin into fibrin degradation products (FDPs),
- Removal of FDPs by the liver and kidneys.
Fibrinolysis is carefully regulated to ensure it doesn’t interfere with necessary clot formation. Inhibitors like plasminogen activator inhibitor-1 (PAI-1) and α2-antiplasmin help to control the fibrinolytic process.
Also Read: How to Stop Bleeding: A Guide to Stopping Bleeding
Factors Affecting Hemostasis
Various factors can influence the hemostatic process. Thus, after learning hemostasis meaning, knowing the factors affecting this process is important to managing bleeding disorders and preventing thrombotic events. These can be divided into factors that promote clotting (procoagulant factors) and those that inhibit clotting (anticoagulant factors). Some of these are discussed as follows:
- Blood Flow: The rate of blood flow can affect platelet adhesion and the concentration of clotting factors at the site of injury.
- Blood Vessel Integrity: The condition of blood vessels, particularly the endothelium, plays a crucial role in hemostasis.
- Platelet Count And Function: Adequate numbers of properly functioning platelets are essential for effective primary hemostasis.
- Clotting Factors: The presence and proper function of all clotting factors are necessary for the coagulation cascade.
- Calcium Levels: Calcium ions are required for several steps in the coagulation cascade.
- Vitamin K: This vitamin is necessary for the production of several clotting factors in the liver.
- Fibrinolytic System: The balance between clot formation and breakdown is crucial for normal hemostasis.
- Temperature: Extreme temperatures can affect enzyme activity in the coagulation cascade.
- pH: The acid-base balance of the blood can influence the activity of clotting factors.
- Medications: Many drugs, including anticoagulants and antiplatelet agents, can significantly affect hemostasis.
First Aid Training Made Easy
Learn essential first aid care from anywhere with our online course
Clinical Significance of Hemostasis
The study of hemostasis has significant clinical implications. This process helps in diagnosing and treating various bleeding and clotting disorders. It’s also crucial for managing patients undergoing surgery or those on anticoagulant therapy.
Disorders of hemostasis can lead to either excessive bleeding or inappropriate clotting, both of which can have serious health consequences.
- Diagnosing Bleeding Disorders: Conditions like hemophilia, von Willebrand disease, and platelet function disorders can be identified through tests of hemostatic function.
- Managing Anticoagulant Therapy: Patients on blood thinners like warfarin or heparin require careful monitoring of their hemostatic function to prevent both bleeding and clotting complications.
- Perioperative Management: Hemostasis also helps in managing bleeding risks during and after surgery.
- Treating Thrombotic Disorders: Conditions like deep vein thrombosis and pulmonary embolism involve inappropriate clot formation and require interventions based on associated principles.
- Developing New Therapies: Research into hemostasis has led to the development of new anticoagulants, antiplatelets, and hemostatic agents.
- Trauma Management: Rapid assessment and management of hemostasis is critical in trauma situations to prevent excessive blood loss.
- Obstetric Care: Understanding hemostasis is important for managing conditions like postpartum hemorrhage.
Recent advances in our understanding of hemostasis have led to improved diagnostic tests and more targeted therapies for disorders of hemostatis. For example, thromboelastography (TEG) and rotational thromboelastometry (ROTEM) are now used to provide a more comprehensive assessment of hemostatic function in real time, allowing for more personalized treatment strategies.
Hemostasis in Action to Keep Blood Flow in Check for Survival!
Hemostasis is a complex process highly tuned to maintain health. From the immediate action of vasoconstriction to the formation of a stable fibrin clot, each phase of the hemostatic process is critical in preventing hemorrhage without invoking excessive coagulation.
As science continues to evolve, diagnostic tools and targeted therapies will be increasingly sophisticated. Hence, clinical improvements relative to hemostasis are reached with a wide range of clinical scenarios.
The fields of study regarding hemostasis have continued to evolve and remain exciting, with discoveries made time after time to provide better management of blood-related disorders and patient care. Moreover, individuals must be aware of all new guidelines and techniques used during any cardiac emergency. For this, they can consider enrolling in a basic life support training course and being responsible citizens of their nation.