CPR, First Aid, BLS, ACLS, PALS certifications.

$119.00 $169.00
| Chapters | CE Credits | Validity | Cost | Duration | ECC | Exam Attempts | Wallet Card |
|---|---|---|---|---|---|---|---|
| 17 | 4.0 – 8.0 | 2 Years | $119.00 | 3-4 Hrs | Compliant | Unlimited | Download/Print/Mail |
Bradycardia is defined as a heart rate of less than 60 beats per minute. Symptomatic bradycardia and the management thereof, is defined as a heart rate less than 50 beats per minute. Causes of bradycardia include:
Symptoms of bradycardia include:
Signs of bracycardia include:
There are 4 types of ECG rhythms associated with bradycardia:
Sinus bradycardia starts in the SA node with decreased rate (<60 beats/min).
First degree AV block is when the PR interval is prolonged (> 0.20 seconds).
2nd Degree AV block type I (Wenckebach-Mobitz I) is when the PR interval becomes increasingly prolonged, R-R intervals are shortened, and a beat (QRS) finally drops
2nd degree AV block Type II (Mobitz II) is when there is no change in the PR interval and than a beat will drop.
3rd degree Av block is a complete heart block where the P wave and QRS complexes are not connected.
Scenario: You are a paramedic who arrives at a house of the patient who has collapsed. The wife tells you that her husband was having difficulty breathing at first, but then grabbed his chest and collapsed.
Assessment:
Interventions:
Management: at the hospital
The following is an algorithm showing management of bradycardia in detail.
If atropine does not work:
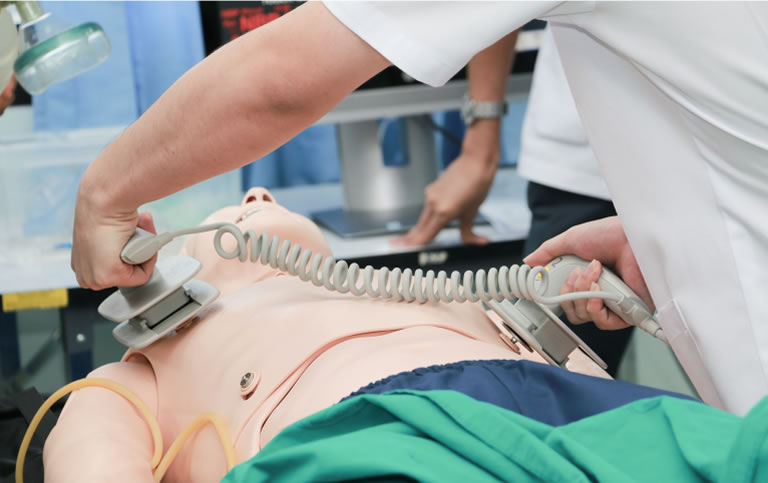
Transcutaneous pacing is crucial to obtain a normal heart rate again if the patient is showing poor perfusion. Even though atropine is the first line treatment for bradycardia, if the patient has severe symptoms of bradycardia or is crashing then it is critical to start Transcutaneous pacing (TCP).
Start TCP right away if the patient:
Once the TCP has started ensure that the heart is getting proper electrical shocks from the pacer. Give analgesics and sedatives to help with pain especially in patients who are alert and awake (might be best to give it before the TCP starts). Make sure to continuously monitor the patient to check if there are any improvements.
REMEMBER: If TCP is ineffective, start infusion of dopamine or epinephrine and get the patient ready for transvenous pacing. Make sure to get professional consultation.
You have completed Chapter XIV. Now you should be able to: