CPR, First Aid, BLS, ACLS, PALS certifications.


$119.00 $169.00
| Chapters | CE Credits | Validity | Cost | Duration | ECC | Exam Attempts | Wallet Card |
|---|---|---|---|---|---|---|---|
| 08 | 4.0 | 2 Years | $119.00 | 3-4 Hrs | Compliant | Unlimited | Download/Print/Mail |
Cardiopulmonary arrest or pediatric cardiac arrest occurs when there is abrupt loss of heart function and blood circulation is terminated due to abnormalities of the heart. Cardiac arrest is uncommon in children and is usually caused by prolonged respiratory distress, failure or shock. Children that have primary cardiac arrhythmias leading to cardiac arrest have very low survival rates so it is important to quickly recognize the problem and provide appropriate treatment.
There are two examples of cardiac arrest that occur in children:
Asphyxia is when there is a lack of oxygen to the body due to difficulty in breathing. Asphyxial arrest is the most common cause of cardiac arrest in children and is due to respiratory failure, shock and cardiopulmonary failure.
Sudden cardiac arrest is uncommon in children and is seen by eh absence of cardiac and respiratory function or by arrest rhythm on the cardiac monitor. Cardiac arrest may be caused by the following problems:
There are 4 examples of cardiac arrest in children:
Asystole or flatline is associated with no cardiac electrical activity, no contraction of the cardiac muscle and no cardiac output. The first step is to ensure that it is an actual asystole and not an error due to improper connection of leads or no power in the unit. Some causes of asystole include:
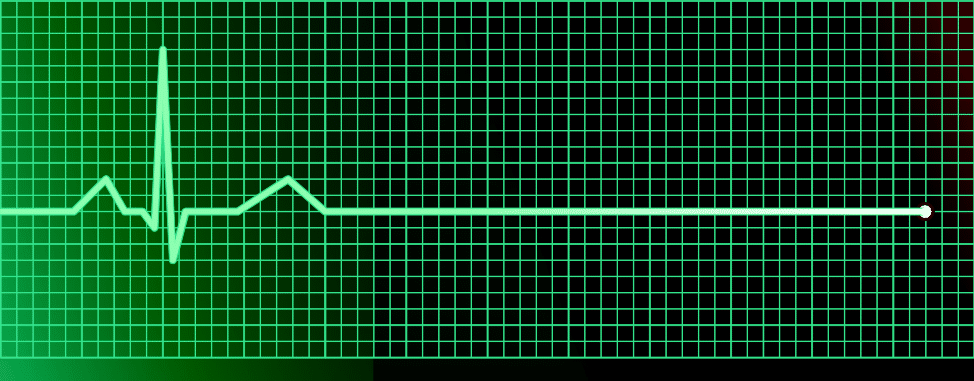
| Signs of Asystole |
|
|
|
|
Ventricular fibrillation (VF) is an arrhythmia, which can cause sudden cardiac arrest. During ventricular fibrillation there is disorganization of electrical activity in the heart and the heart has stopped pumping. VF is common in children and has the following causes:
| Causes of VF |
|
|
|
|
|
|
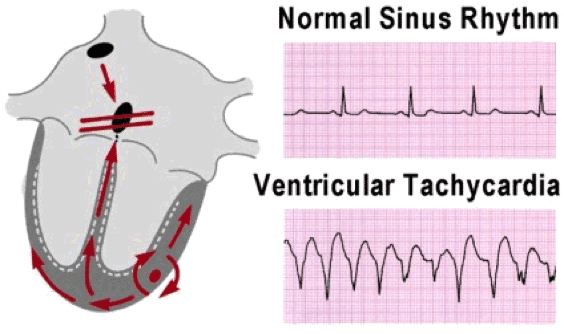
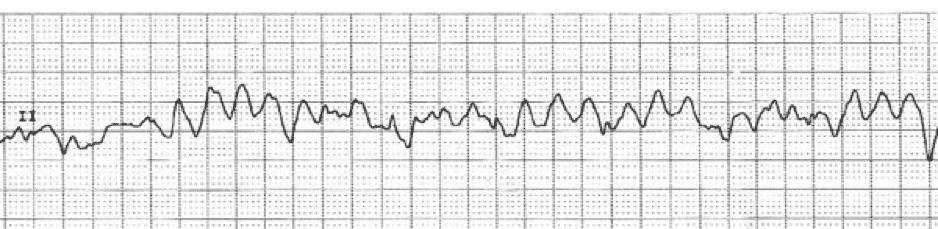
VF does not have an identifiable ECG waveform. Earlier waveforms show a “coarse VF,” but after few minutes the waveforms are much smaller and show a “fine VF.”
Ventricular tachycardia (V-tach or VT) is a fast heart rhythm from the ventricles of the heart. VT can lead to VF and cause sudden death of the patient. A pulseless VT has no cardiac output causing no pulse and results in cardiac arrest. The causes of pulseless VT are:
| Causes of VT |
|
|
|
|
|
|
change pic 9
Pulseless electrical activity (PEA) is lack of palpable pulse or cardiac contraction even with an organized cardiac electrical activity. PEA presents with prolong PR and QT intervals, AV dissociation or complete heart block.
PEA can be caused by many factors and are represented as H’s and T’s:
| H’s | T’s |
| Hypovolemia | Tension pneumothorax |
| Hypoxia | Tamponade |
| Hydrogen ion (acidosis) | Toxins |
| Hyper-/hypokalemia | Thromobosis (pulmonary) |
| Hypothermia | Thrombosis (coronary) |
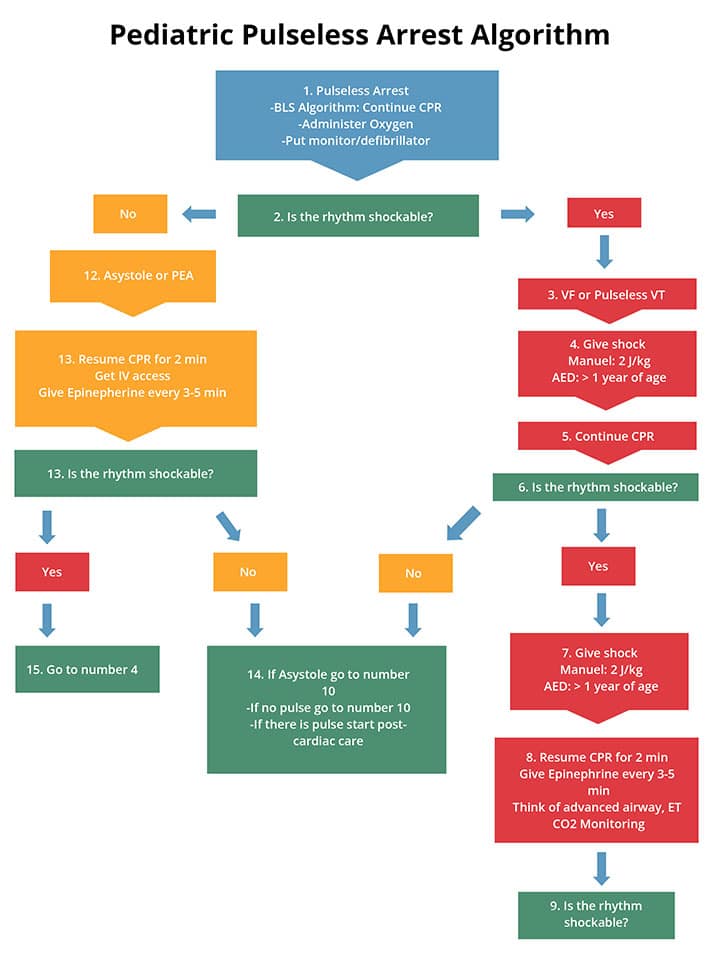
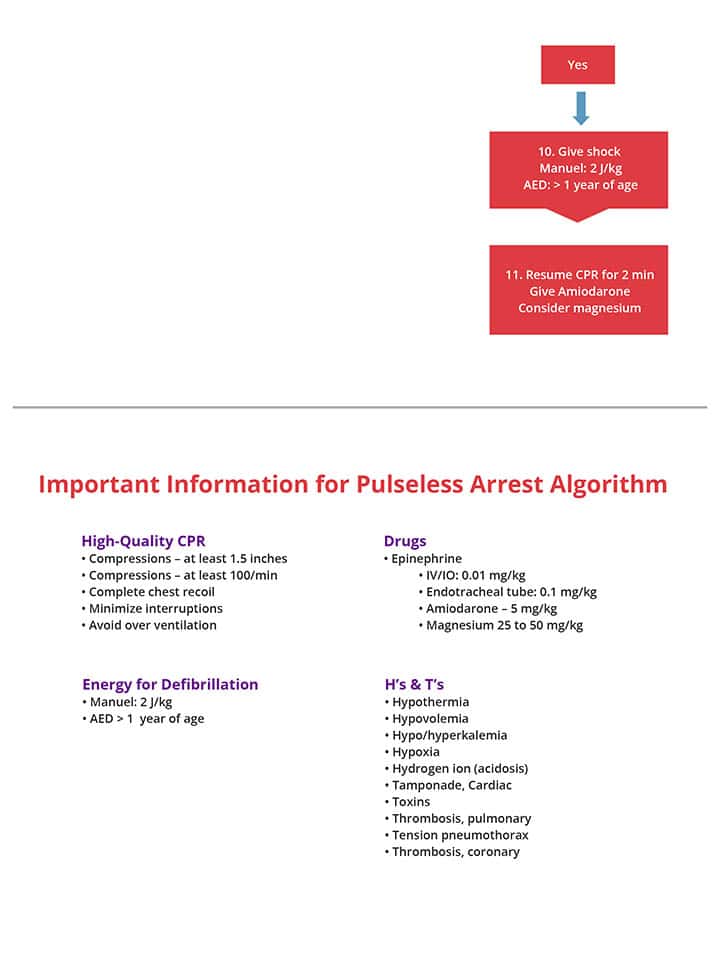
The most important component in the management of cardiac arrest is activating the EMS and implementing high-quality CPR continuously, for infants compression depth is 1.5 inches, for children (1+ years) it’s 2 inches. There are different steps in order to treat a child with VT/VF and those with asystole or PEA.
The following is the algorithm which shows the management of cardiac arrest of children: