CPR, First Aid, BLS, ACLS, PALS certifications.

$119.00 $169.00
| Chapters | CE Credits | Validity | Cost | Duration | ECC | Exam Attempts | Wallet Card |
|---|---|---|---|---|---|---|---|
| 17 | 6.0 | 2 Years | $119.00 | 3-4 Hrs | Compliant | Unlimited | Download/Print/Mail |
Acute coronary syndrome or ACS is defined as a sudden, reduced blood flow to the heart. ACS is seen in ST-segment elevation myocardial infarction (STEMI), non-ST-segment elevation myocardial infarction (NSTEMI) or unstable angina. Myocardial ischemia occurs when there is not enough blood supply to the heart muscle and that results from coronary artery disease (CAD). ACS is usually caused by atherosclerosis and coronary thrombosis, but can also be associated with cocaine use. Other conditions that cause ACS include:
The symptoms associated with ACS include:
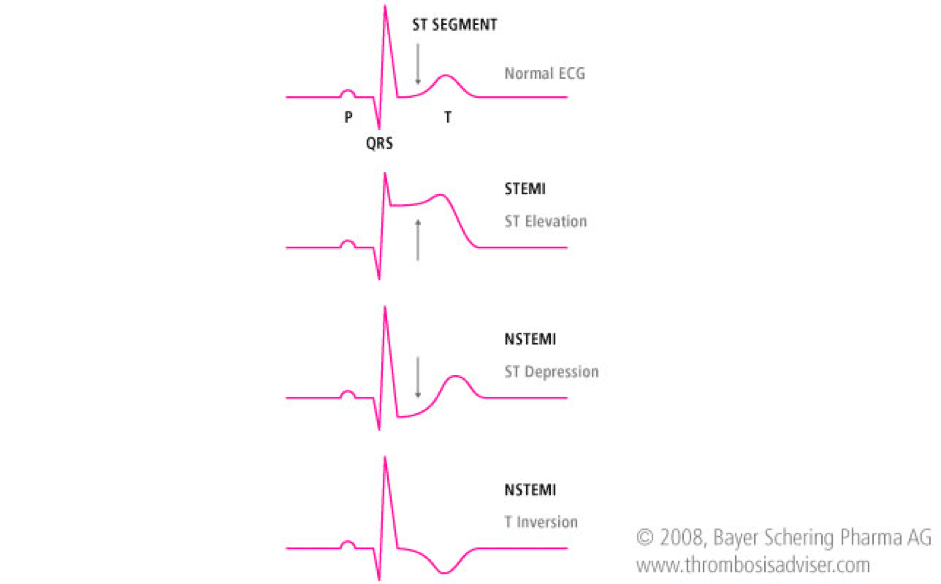
ST-Segment Elevation Myocardial Infarction (STEMI) is an elevation > 1mm in 2 or more contiguous or greater than 2 mm in leads V2 and V3.
Unstable Angina (UA) or Non ST-Elevation Myocardial Infarction (NSTEMI) is a depression ≥0.5 mm or greater T-wave inversion.
Low Risk Unstable Angina (UA) is an ST segment deviation of <0.5 mm or T wave inversion of 2 mm. Patients may also have normal ECGs.
Scenario: A 70-year patient comes to the hospital and is complaining of chest pain radiating to his arm and he seems very anxious and out of breath.
Assessment:
Interventions:
Management:
Treatments which are used in ACLS algorithm for ACS are:
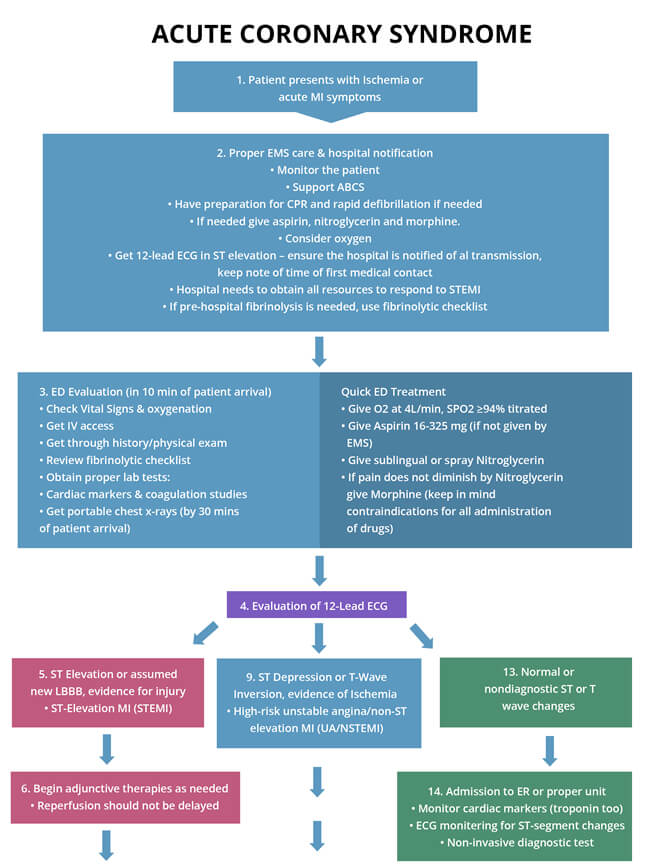
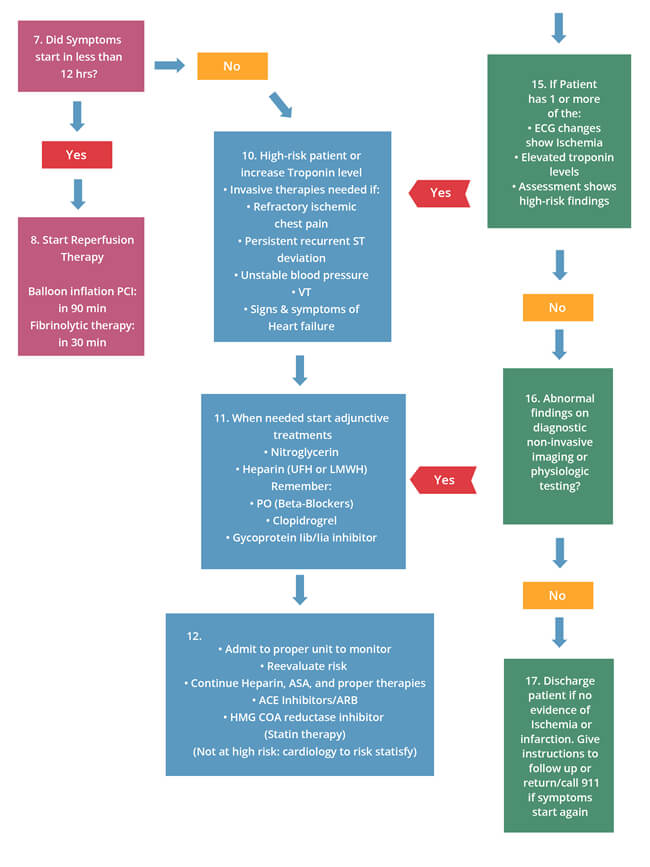
The following is an algorithm that shows management of ACS in detail: