CPR, First Aid, BLS, ACLS, PALS certifications.


$119.00 $169.00
| Chapters | CE Credits | Validity | Cost | Duration | ECC | Exam Attempts | Wallet Card |
|---|---|---|---|---|---|---|---|
| 08 | 4.0 | 2 Years | $119.00 | 3-4 Hrs | Compliant | Unlimited | Download/Print/Mail |
Respiratory distress can lead to respiratory failure in children that can be life threating and can quickly lead to death. Prompt recognition and management of respiratory distress and failure in infants and children is one of the key components of PALS. Respiratory distress is when the rate and effort of breathing is increased and there are changes seen in airway sounds, skin color and mental status. Respiratory distress can quickly lead to respiratory failure, where there is inadequate oxygenation, ventilation or both and can quickly lead to cardiac arrest.
Lung of a child in respiratory failure and needs respirator for assist ventilation |
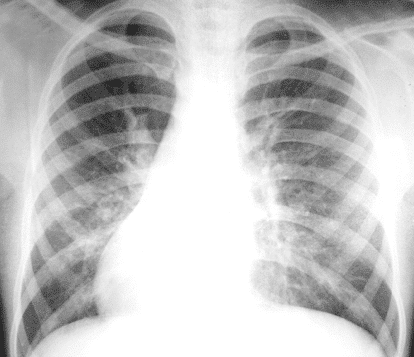
Lung of a child with Respiratory distress syndrome and left sided pneumothorax |
Hypoxemia or inadequate oxygenation and hypercarbia or inadequate ventilation can lead to respiratory distress and failure. It is important to note that oxygen consumption in infants is 6 to 8 mL/kg per minute, while in an adult it is 4 mL/kg per minute. A pulse oximetry helps indicate if there is decreased oxyhemoglobin saturation in the blood. A SpO2 <94% = hypoxemia. Tissue hypoxia could also be a cause of hypoxemia. It is important to recognize the signs of hypoxia to help distinguish between tissue hypoxia and hypoxemia. The following are signs of tissue hypoxia:
Increased PaCO2 in the blood indicated inadequate alveolar ventilation or hypercarbia. Hypercarbia is more severe, but is harder to detect. The following are signs of hypercarbia:
| Upper Airway Obstruction | |
| Anatomy | Obstruction in the nose, pharynx, or larynx |
| Causes |
|
| Signs and Symptoms |
|
| Management | Management of all upper airway obstruction includes:
|
Specific causes of upper airway obstruction include croup and anaphylaxis.
Croup is a condition where the upper airway is affected due to an acute viral infection. Symptoms include barking cough, stridor and hoarseness. Treatment of croup can vary due to the severity of the disease. Management of croup includes the following:
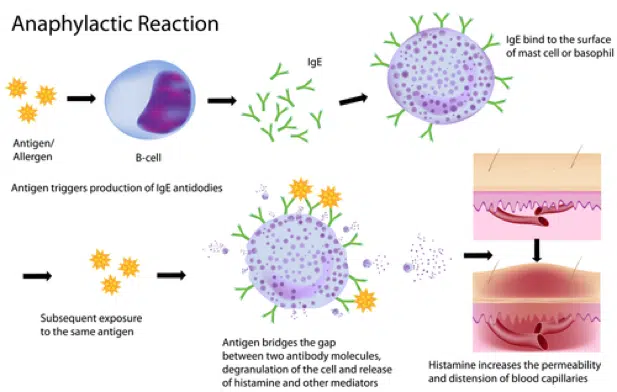
Anaphylaxis is a type I hypersensitivity allergic reaction that can causes intense bronchoconstriction in which the patient may stop breathing. The following table shows the actions needed for the treatment of anaphylaxis.
| Treatment |
| Give IM epinephrine through the autoinjector – depends on how severe the problem is |
Think of using endotracheal intubation if there is bronchospasm/wheezing – give albuterol through inhaler or by nebulizer For severe bronchospasm give nebulizer continuously |
| Prepare for ET intubation |
If the child has hypotension:
|
| Give methylprednisolone or corticosteroids and diphenhydramine |
| Lower Airway Obstruction | |
| Anatomy | Obstruction in lower trachea, bronchi or bronchioles
|
| Causes |
|
| Signs and Symptoms |
|
| Management | Management of all lower airway obstruction includes:
|
Specific causes of lower airway obstruction include asthma and bronchiolitis.
Bronchiolitis is inflammation of the bronchioles with coughing, shortness of breath and wheezing. Management of bronchiolitis includes the following:
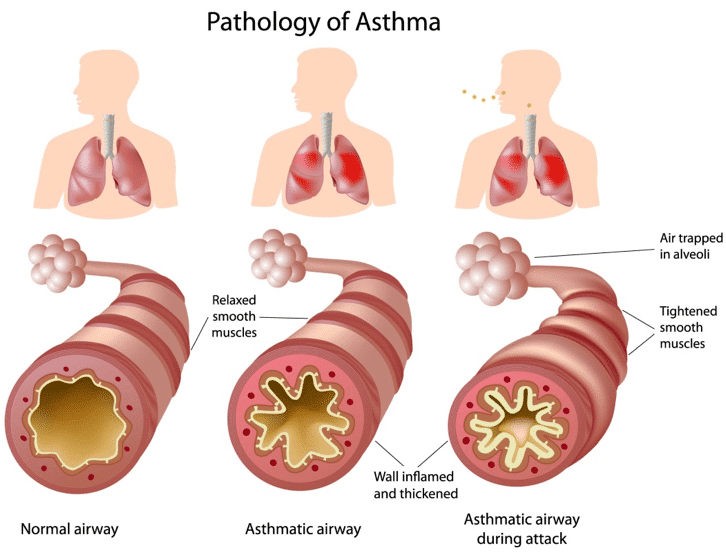
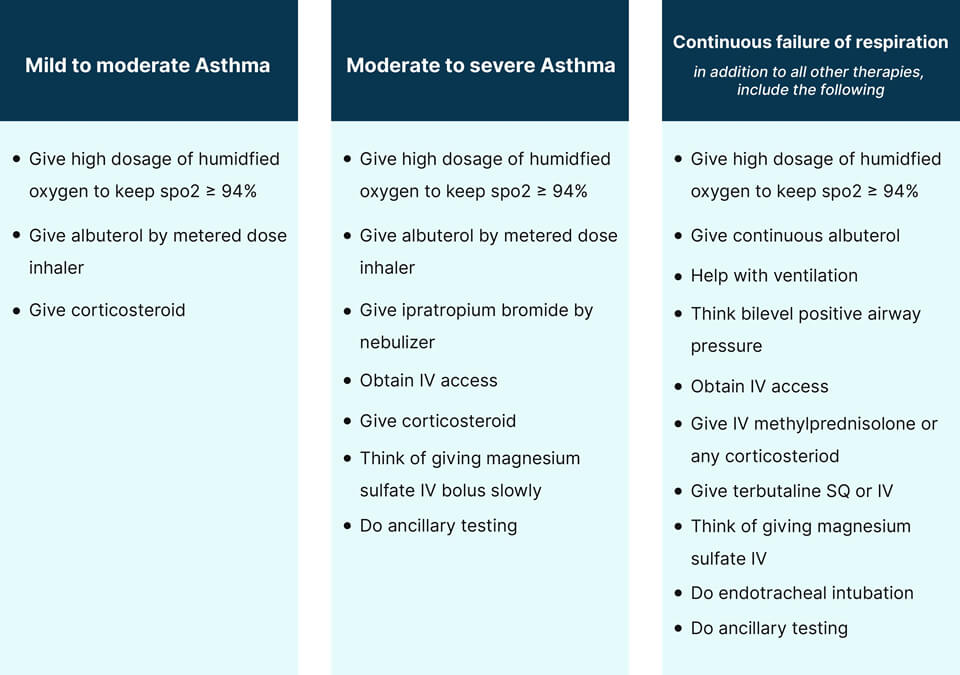
Asthma is a chronic inflammatory disease of the airway with symptoms of coughing, shortness of breath, wheezing and tightness of the chest. The following table illustrates the management of asthma.
| Lung Tissue Disease | |
| Anatomy | Clinical conditions with the lungs |
| Causes |
|
| Signs and Symptoms |
|
| Management | Management of all tissue lung disease includes:
|
Specific causes of lung tissue disease include pneumonia, chemical pneumonitis, aspiration pneumonitis, cardiogenic pulmonary edema and noncardiogenic pulmonary edema (ARDS).
Pneumonia is inflammation of the alveoli of the lungs due to infection by bacteria, viruses, fungi and parasites. Pneumonia presents with fever, chest pain, cough, difficulty in breathing. The management of pneumonia includes:
Chemical pneumonitis is inflammation of the lungs caused by breathing in toxic substances. Toxic substances include dust, fumes, irritant gases, hydrocarbons. Management of chemical pneumonitis is done by:
Aspiration pneumonitis is inflammation of the lungs caused by content of the stomach such as stomach acid and enzymes. For treatment of aspiration pneumonitis consider the following options:
Cardiogenic pulmonary edema occurs when there is an accumulation of fluid in the lung interstituim and alveoli because of elevated pulmonary capillary pressure. Most common cause of cardiogenic pulmonary edema is congestive heart failure and acute myocardial dysfunction. Management of cardiogenic pulmonary edema includes:
Acute respiratory distress syndrome is inflammation of the lung parenchyma causing difficulty in breathing, hypoxemia and multiple organ failure. ARDS as defined by the American Heart Association is, acute onset, PaO2/FiO2 <300, bilateral infiltrates on chest x-ray, and no evidence for a cardiogenic cause of pulmonary edema. Management of ARDS includes:
| Disordered Control of Breathing | |
| Anatomy | Problems associated with the respiratory system |
| Causes |
|
| Signs and Symptoms |
|
| Management | Management of disordered control of breathing includes:
|
Specific causes of disordered control of breathing include increased intracranial pressure (ICP), poisoning or drug overdose, and neuromuscular diseases.
Increased intracranial pressure can be caused by:
Proper management of respiratory distress or failure due to increased ICP includes:
Poisoning and drug overdose is one of the most common and frequent causes of respiratory distress in infants and children. The following actions must be taken to treat this type of respiratory distress.
Neuromuscular disease is broad term that is given to various diseases that impair muscle control and causes spasticity or paralysis. Children with neuromuscular diseases which affect respiration have the following symptoms:
For management of neuromuscular disease in children complete the ABC assessment, which includes supporting the airway, breathing and circulation.