According to the American College of Cardiology, about 2 in every 50 U.S. high schools will see a sudden cardiac arrest (SCA) each year. While the number covers all students, the risk often shows up most dramatically in athletes. That’s because adolescence is when hidden heart conditions are more likely to surface under the strain of sports and intense activity.
CPR stands for Cardiopulmonary Resuscitation. It isn’t just a vague lifesaving “system.” It’s a hands-on backup for the heart and lungs when they fail. It mimics the natural system temporarily. Chest compressions force blood to circulate, whereas rescue breaths or oxygen keep vital organs alive until professional help arrives.
So what does CPR really mean, and why should you know it? Let’s find out!
What Does CPR Stand For in 3 Words?
CPR breaks down into three simple but powerful words that explain exactly what this technique does. CPR means Cardiopulmonary Resuscitation. Each letter is important in emergency care. “Cardio” means heart, “pulmonary” means lungs, and “resuscitation” means resuscitating someone or reviving them from death. Here’s the science behind each term:
- Cardio
Cardio relates to heart function and blood circulation throughout the body. During cardiac arrest, the heart stops pumping blood to vital organs. Without blood flow, organs begin dying within minutes. CPR chest compressions manually squeeze the heart, forcing blood through the circulatory system.
- Pulmonary
Pulmonary focuses on lung function and oxygen delivery. When someone stops breathing, their blood oxygen levels drop rapidly. Brain cells begin dying without an adequate oxygen supply. CPR rescue breaths deliver fresh oxygen directly into the lungs. It maintains oxygen levels in the bloodstream. The effectiveness depends on a patent airway, and sometimes breaths don’t work if there’s an obstruction or improper seal.
- Resuscitation
Resuscitation means restoring life or consciousness in someone who appears dead or unresponsive. Clinically, it refers to the emergency steps taken when the heart or lungs fail. It involves actively restarting or sustaining circulation and oxygen delivery so that the brain and other vital organs don’t shut down. In practice, this can involve chest compressions, rescue breathing, defibrillation, or advanced interventions like airway management and medications. Together, these measures buy time until the body’s natural systems can recover or a medical team can take over.
Career Relevance
Knowing CPR isn’t just for emergencies at home. In the U.S., certification is required for many healthcare jobs, childcare workers, teachers, lifeguards, and even workplace safety compliance roles. It’s a practical skill that employers often demand.
Legal Protections
Many hesitate to act, fearing legal risk. But Good Samaritan Laws protect bystanders who give CPR in good faith. These laws encourage action by shielding rescuers from liability because saving a life matters more than perfection.
CPR History Timeline
CPR didn’t appear overnight. It evolved through decades of trial, error, and breakthrough.
1950s: Peter Safar and James Elam proved that chest compressions plus mouth-to-mouth ventilation could keep oxygen and blood moving. Their work changed the understanding of emergency care.
1960: The American Heart Association officially adopted CPR and began training both medical staff and the public. This turned CPR into a community-wide skill instead of just a hospital intervention.
1980s–1990s: Automated External Defibrillators (AEDs) became available outside hospitals. For the first time, ordinary people could deliver lifesaving shocks before paramedics arrived.
Today: CPR and AED training are standard across schools, workplaces, and communities. The role of bystanders is now seen as the first and most crucial link in the chain of survival.
What Are the 7 Steps of CPR?
Step 1: Check Responsiveness
Tap the person’s shoulders and yell, “Are you okay?” This way, you won’t give CPR to someone who is just unconscious but breathing normally. Listen for the sounds of normal breathing. Check for chest movement. If the person doesn’t react and isn’t breathing normally, start CPR. Don’t take time to check for a pulse unless you have been trained. Checking a pulse can waste critical seconds. Look for signs of life and initiate compressions if in doubt.
Step 2: Call for Help
Dial 911 immediately and request an AED if available. Research conducted by AHA indicates that CPR performed by bystanders increased to 44% in women and 40% in men with 911 operator guidance. If there are other people around, delegate specific responsibilities: one calls 911, the other searches for an AED, while you initiate CPR. You can also direct someone to wait outside for EMS to speed their arrival and ask others to keep the area clear so rescuers have space to work.
Step 3: Position the Person
Put the victim on his or her back on a hard surface. Gently tilt the head back and lift the chin to open the airway. If you notice something in the mouth that can be easily taken out (such as food or gum), remove it gently. Positioning is important to provide effective chest compressions and an unobstructed airway passage.
Step 4: Position Your Hands.
Put the heel of one hand in the middle of the chest, just between the nipples. Put your other hand on top of it, with your fingers interlaced. Keep your fingers raised off the chest wall. Your shoulders should be right above your hands, with arms straight and locked.
Step 5: Start Chest Compressions
Push firmly and rapidly at least 2 inches deep at 100-120 compressions per minute. Use the rhythm of songs like “Stayin’ Alive” or “Baby Shark” to keep your pace correct. Permit full chest recoil between compressions. Count out loud to keep your pace steady. It’s important to know that rib fractures are common during CPR, and that’s okay. Bones can heal, but brain damage from lack of oxygen cannot.
Step 6: Administer Rescue Breaths
Following 30 compressions, tilt the head back, lift the chin, and administer 2 rescue breaths. The chest should rise visibly with each breath. Form a seal over the person’s mouth with your hand, closing their nose. Each breath should be taken for approximately 1 second. Not a trained breath giver? No worries, hands-only CPR (only compressions) is still life-saving.
Step 7: Continue Cycles
Repeat 30 compressions followed by 2 breaths until emergency services arrive, an AED is available to use or the person begins breathing normally. Switch with another trained person every 2 minutes to prevent fatigue. Don’t stop CPR unless the person starts breathing normally or emergency services take over.
Real-Life Rescue (2025)
In California (2025), an assistant soccer coach collapsed during class and went into cardiac arrest. The high school’s athletic trainer arrived within two minutes, hooked up an AED, delivered a shock while chest compressions continued, and revived him before EMS arrived.
Is CPR Always 30 to 2?
The 30:2 ratio (30 compressions and 2 breaths) is the usual guideline for most CPR cases, yet it’s not absolute. The ratio may be modified based on the person’s age and the number of people performing CPR. Here is a summary of the variations,
- Adult CPR Ratios
For adults, the recommended ratio continues to be 30 compressions to 2 breaths for single rescuers. Two-rescuer CPR, however, also uses the same 30:2 ratio, as opposed to pediatric guidelines. The consistency makes training easier and decreases confusion during stressful emergencies.
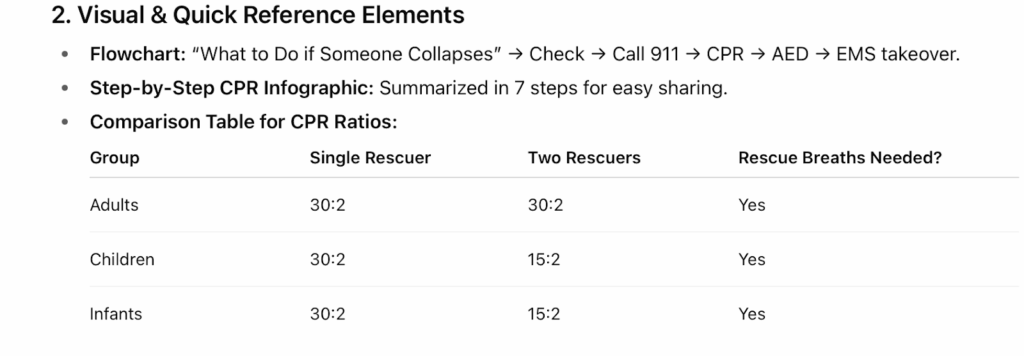
- Pediatric Variations
Children have different ratios because of their smaller stature and divergent physiology. Single rescuer pediatric CPR employs 30:2, but two-rescuer pediatric CPR becomes 15:2 for more respiratory effort at a higher frequency. Younger kids have less lung capacity and need oxygen more often. Babies require a special technique: use two fingers, or thumbs, with hands around the chest (if two individuals are available). If you’re ever unsure whether to treat a child as an infant, treat them as a child. This clears up a common confusion and ensures adequate compressions.
What Is the Golden Rule of CPR?
The golden rule of CPR focuses on a single key idea: “Push hard, push fast, don’t stop.” According to the American Heart Association (AHA), survival rates more than doubled when compressions were performed at the recommended depth and speed without interruptions. It is the most important principle of delivering high-quality chest compressions continuously. Here’s how you can put the golden rule into practice:
- Quality Over Quantity
Successful CPR involves compressions that are at least 2 inches (5 cm) deep in adults. If you are not reaching that 2-inch depth, the CPR may not be effective. Shallow compressions cannot produce sufficient blood flow to the vital organs, especially the heart and brain. Don’t be afraid of pressing too hard since sufficient depth is needed for survival. Make sure the depth is not more than 2.4 (6 cm) since it causes rib fractures, lung puncture, laceration of the liver, and injury to the heart itself.
- Consistency is Key
Keeping at 100-120 compressions per minute allows for the best blood flow. Initiating bystander CPR within a 10-minute time frame increases chances of survival and lessens brain injury. Utilize a metronome app or time with the rhythm of a song to keep up the correct rhythm. An example is doing compressions to “Cecilia” while being trained in CPR so that muscle memory is related to the rhythm.
- Reduce Interruptions
With each break in chest compressions, the chances of survival for the victim decrease. Continuous, high-quality compressions are the golden rule of good resuscitation. However, make sure to keep pauses under 10 seconds, whether for rescue breaths or applying an AED. Blood pressure decreases to zero within a few seconds of ceasing compressions.
What Does CPR Mean in Different Contexts?
CPR’s meaning differs according to the emergency, the person’s condition, and the resources present. Here’s a short rundown of various settings to assist you in modifying your response to give the best possible care.
Drowning Victims
Near-drowning victims need different CPR strategies. The initial issue in drowning situations is oxygen deprivation, not cardiac arrest. The brain must be supplied with oxygen immediately to avoid irreversible injury. Thus, start with two rescue breaths followed by chest compressions.
Drug Overdose Situations
Opioid overdoses may require CPR combined with naloxone administration. A recent study from the AJMC shows increasing overdose-related cardiac arrests, making this combination approach increasingly important. If unsure whether opioids are involved, CPR should still be started. Focus on chest compressions while others administer naloxone if available.
Pregnancy Considerations
If the cardiac arrest occurs after 20 weeks of pregnancy, place a wedge or rolled towel under the right hip, tilting the body 15–30° to the left. This prevents the uterus from compressing major blood vessels and reduces shock risk.
Traumatic Cardiac Arrest
Trauma victims can sometimes need modified CPR techniques based on their injury. For example, if the victim has an injury to their spine, you must continue manual spinal stabilization with jaw-thrust rather than head-tilt. However, if the victim is suffering from heavy bleeding, you must treat it with appropriate tourniquet application before initiating compressions.
Read More: Venous Bleeding vs. Artery Bleeding: Overview & Treatment
What is Proper Body Mechanics for CPR?
Proper positioning prevents ineffective CPR and prevents injury to you during prolonged resuscitation attempts. Inadequate positioning causes ineffective compressions and rescuer fatigue. Now, how do you keep your posture aligned to prevent that? Let’s look at some strategies,
- Rescuer Positioning
Kneel next to the chest of the victim with your knees in close proximity to their body. This stance ensures stability and enables you to utilize the weight of your body efficiently for compressions. Kneeling or standing on a stool/taboret enables rescuers to perform effective compressions for around 2 minutes, but standing on the ground only lasts for approximately 1 minute due to strain and compromised elbow/back support. Try not to kneel too far to minimize compression efficiency.
- Hand Placement
Position the heel of your dominant hand at the bottom half of the breastbone. Your second hand is placed on top with fingers intertwined and raised off the chest. Valid hand position directs force to the strongest location of the chest.
- Body Alignment
Keep your shoulders in line over your hands with straight, locked arms. This position distributes your body weight directly through your arms to produce effective compressions. Bend at the hips rather than the back to ensure proper posture. Keep arms straight and don’t bend elbows.
- Fatigue Management
Switch with another rescuer every 2 minutes to avoid fatigue-induced compression quality loss. Compressions have been found to decrease significantly after 2 minutes of uninterrupted CPR, according to research. Don’t wait until you are tired before switching positions.
What are the Types of CPR Techniques?
Different CPR approaches serve specific emergencies and rescuer skill levels. Therefore, you need to choose the most appropriate technique for each scenario you encounter. Let us explore the types of CPR techniques,
- Conventional CPR
The traditional mouth-to-mouth with chest compressions is still the standard among trained rescuers. This technique offers both oxygenation and circulation to the vital organs. Traditional CPR is most effective when conducted by trained persons who are at ease with rescue breathing.
- Hands-Only CPR
One or two rescue breaths with chest compressions are effective for adult cardiac arrest victims. According to studies, hands-only CPR is as effective even when provided by untrained bystanders. The simplified process eliminates obstacles that keep individuals from assisting.
- Compression-Only CPR
This type is a simplified method that only involves chest compressions. Compression-only CPR is especially helpful in cases where mouth-to-mouth rescue breathing is not possible or safe. Compression-only CPR is effective for short durations until expert assistance is provided.
- AED-Assisted CPR
Automated External Defibrillators support CPR by scanning heart rhythms and providing electric shocks when needed. Combined AED and CPR strategies have better survival outcomes in witnessed cardiac arrest. Voice directions given by AEDs walk untrained individuals through proper procedures.
Read More: CPR and AED Training: Why Both Are Critical for Healthcare Providers
What Are the Most Common CPR Myths vs Facts
The biggest obstacle to CPR is hesitation, often fueled by myths. Here’s where people get it wrong:
Myth: CPR always revives someone immediately.
Fact: CPR doesn’t restart the heart. It actually buys time. It keeps blood and oxygen moving until a defibrillator or trained medical care restores a normal rhythm.
Myth: You could cause more harm than good.
Fact: Broken ribs happen often, and they heal. Permanent brain injury from no oxygen does not. Doing CPR, even imperfectly, gives someone a chance they wouldn’t otherwise have.
Myth: CPR is only for trained professionals.
Fact: Hands-only CPR has proven that anyone can save a life. Pushing hard and fast on the chest doubles or triples survival chances, even without breaths.
When NOT to Perform CPR
Although CPR is almost always the right move, there are clear exceptions:
- DNR Orders: A Do Not Resuscitate order is a legal medical directive that must be honored. Attempting CPR in these cases goes against the patient’s wishes.
- Obvious Death: If there are unmistakable signs of death, such as rigor mortis, decomposition, or injuries incompatible with life, CPR should not be attempted.
- Unsafe Environment: Rescuers shouldn’t become victims. If the scene is too dangerous, wait until it’s secure before starting CPR.
Turn CPR Awareness Into Life-Saving Action
Learning what does CPR stand for is just the beginning of your lifesaving journey. Recall the golden rule, “Push hard, push fast, don’t stop”, in order to provide blood circulation and oxygenation until the professionals arrive. Cardiopulmonary Resuscitation represents empowerment, preparedness, and the ability to act decisively when someone needs you most. Take action today by enrolling in a certified online CPR course. Gain the knowledge, skills, and confidence to respond effectively from the comfort of your home.
FAQs
- What is the correct CPR ratio for adults?
For adults, the correct CPR ratio is 30 compressions to 2 breaths. Each compression should be at least 2 inches deep and at a pace of 100–120 per minute, ensuring proper circulation until professional help arrives.
- How long should CPR be performed before stopping?
You keep going until one of three things happens: the person revives, trained medical responders take over, or you physically can’t continue. Stopping early lowers survival odds, so persistence is often the difference-maker.
- Is CPR different for infants and children?
Yes, kids aren’t just small adults. Children require 30:2 if you’re alone, or 15:2 with two rescuers. Infants need gentler compressions, two fingers or thumbs, because their bones and lungs are far more delicate.
- Can CPR be done without rescue breaths?
Yes. Hands-only CPR involves continuous chest compressions without breaths. It has been shown to improve survival in adult sudden cardiac arrest, especially outside hospitals. It’s easier for untrained bystanders and still provides critical blood flow to the brain and heart.
- What certifications are needed for CPR in healthcare?
Healthcare workers typically complete Basic Life Support (BLS) certification from the American Heart Association or the Red Cross. Many also pursue Advanced Cardiac Life Support (ACLS), depending on their role. These certifications must be renewed regularly to stay current.